Overview

Tendinopathy
Types of Tendinopathy
- Definition: Refers to the acute inflammation of a tendon.
- Causes: Often results from sudden overload or acute injury.
- Symptoms: Pain, swelling, and warmth around the affected tendon.
- Definition: Describes the chronic degeneration of a tendon without significant inflammation.
- Causes: Typically due to repetitive strain or overuse, leading to micro-tears in the tendon.
- Symptoms: Persistent pain, stiffness, and reduced strength. Unlike tendinitis, swelling is less pronounced.
Common Sites of Tendinopathy
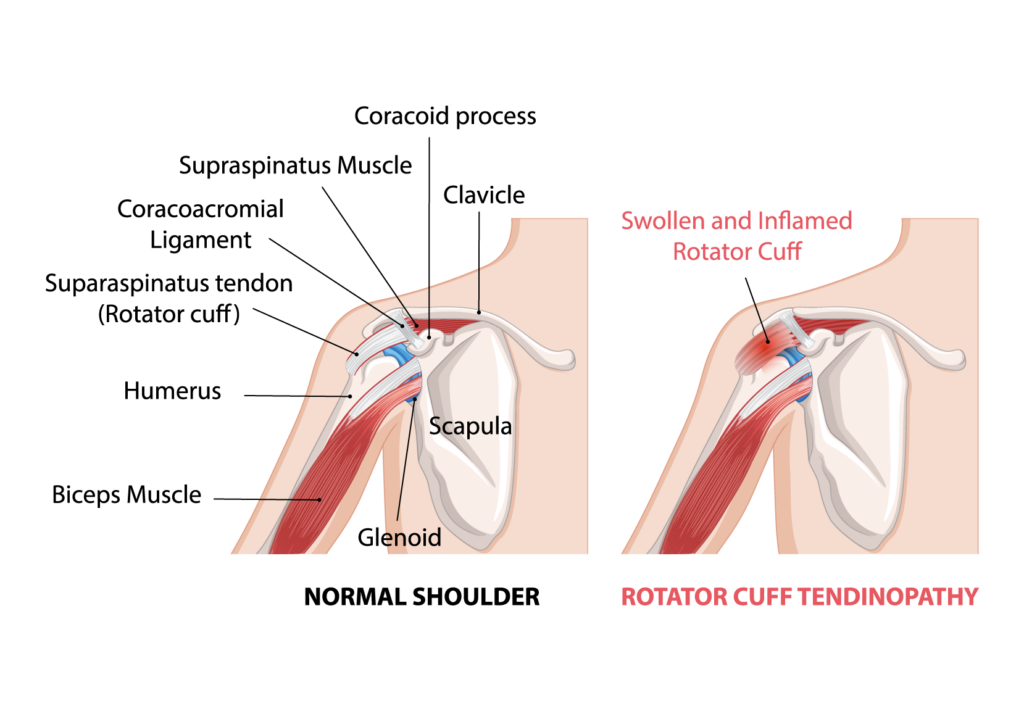
1. Rotator Cuff Tendinopathy:
– Affects the tendons of the shoulder, causing shoulder pain and weakness.
2. Lateral Epicondylitis (Tennis Elbow):
– Involves the tendons on the outside of the elbow, leading to pain and tenderness.
3. Medial Epicondylitis (Golfer’s Elbow):
– Affects the tendons on the inside of the elbow, causing pain and tenderness.
4. Patellar Tendinopathy (Jumper’s Knee):
– Affects the tendon connecting the kneecap to the shinbone, common in athletes involved in jumping sports.
5. Achilles Tendinopathy:
– Involves the tendon connecting the calf muscles to the heel, leading to heel pain and stiffness.
Causes and Risk Factors
- Overuse and Repetitive Movements: Repeated stress on a tendon without adequate rest can lead to micro-damage and degeneration.
- Age: Tendons become less flexible and more prone to injury with age.
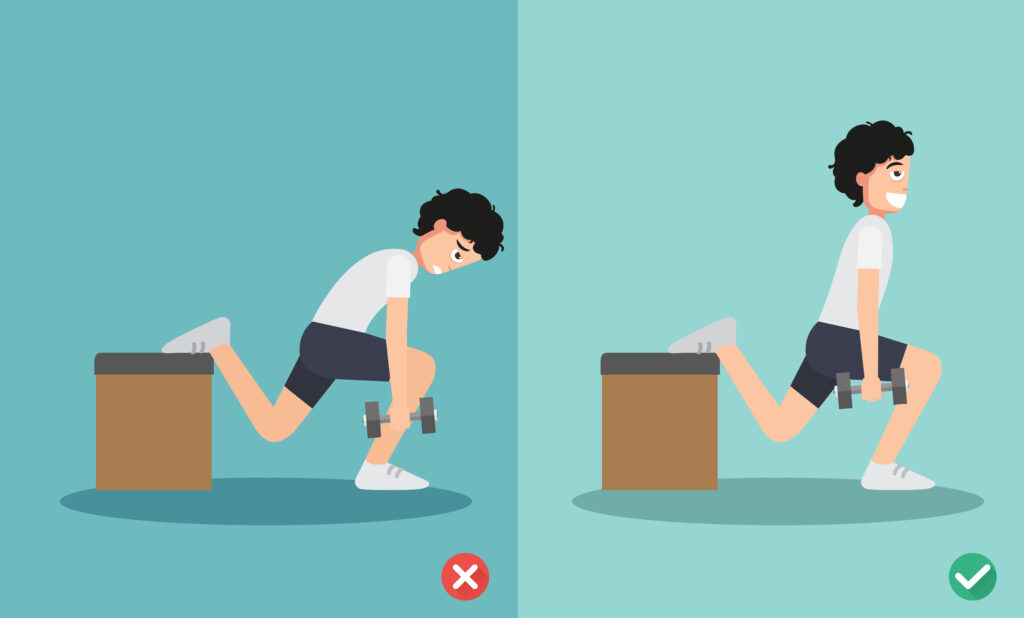
- Poor Technique: Improper form during physical activities can increase tendon stress.
- Inadequate Conditioning: Weak muscles can place additional strain on tendons.
- Sudden Increase in Activity Level: Rapidly intensifying physical activity without proper progression can lead to tendinopathy.
- Genetic Factors: Some individuals may have a genetic predisposition to tendon injuries.

Diagnosis
Diagnosis of tendinopathy typically involves:
1. Medical History and Physical Examination:
– Evaluating symptoms, activity level, and occupation.
– Physical examination to assess pain, tenderness, and range of motion.
2. Imaging Studies:
– **Ultrasound**: Can detect tendon thickening, tears, and inflammation.
– **MRI**: Provides detailed images of tendon structure and any degenerative changes.
Treatment Options
1. Non-Surgical Treatments:
– Rest and Activity Modification: Reducing or avoiding activities that exacerbate symptoms.
– Physical Therapy: Exercises to strengthen the tendon and surrounding muscles, improve flexibility, and correct biomechanics.
– Pain Management: Use of NSAIDs (non-steroidal anti-inflammatory drugs) to relieve pain. Note: Tendinosis is not primarily inflammatory, so NSAIDs may have limited efficacy.
– Orthotics and Braces: Supportive devices to alleviate stress on the affected tendon.
– Extracorporeal Shock Wave Therapy (ESWT): Uses sound waves to promote healing of chronic tendinopathies.
2. Injections:
– Corticosteroids: May provide short-term pain relief but should be used cautiously due to potential tendon weakening.
– Platelet-Rich Plasma (PRP): Involves injecting concentrated platelets to promote healing.
3. Surgical Intervention:
– Considered when conservative treatments fail.
– Surgery may involve removing damaged tissue or stimulating healing through different surgical techniques.
Prevention Strategies
– Gradual Increase in Activity: Avoid sudden increases in intensity or duration of exercise.
– Proper Technique and Equipment: Ensure correct form and use appropriate equipment for activities.
– Strength and Flexibility Training: Regularly engage in exercises to strengthen muscles and improve tendon flexibility.
– Adequate Rest and Recovery: Allow time for tendons to recover between activities.