Overview
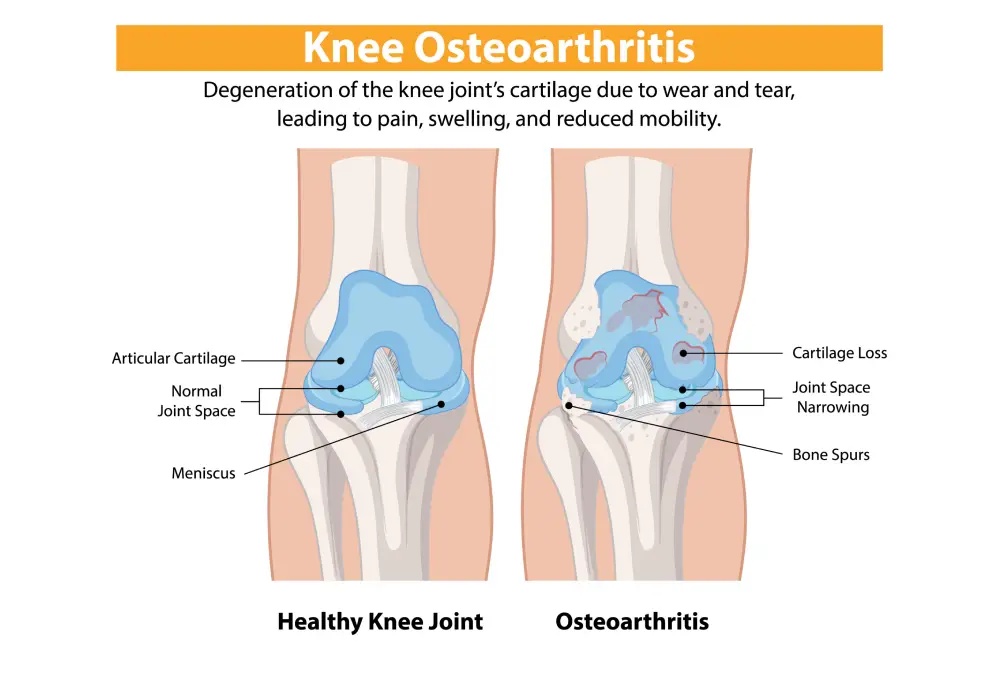
Knee Osteoarthritis
Knee osteoarthritis (OA) is a degenerative joint disease characterized by the breakdown of cartilage, leading to pain, stiffness, and decreased function. It is a common condition, particularly in older adults. Here are key aspects of knee osteoarthritis
Causes and Risk Factors:
- Age: The risk increases with age.
- Gender: Women are more likely to develop OA than men.
- Obesity: Excess weight puts additional stress on knee joints.
- Genetics: Family history can play a role.
- Joint Injuries: Previous knee injuries can increase the risk.
- Repetitive Stress: Occupations or activities that place repeated stress on the knees.
Symptoms:
- Pain: Typically worsens with activity and improves with rest.
- Stiffness: Especially after periods of inactivity or in the morning.
- Swelling: Due to inflammation in the joint.
- Decreased Range of Motion: Difficulty in fully bending or straightening the knee.
- Crepitus: A grating sensation or sound during joint movement.

Diagnosis:
- Clinical Evaluation: Includes medical history and physical examination.
- Imaging: X-rays can show joint space narrowing, bone spurs, and other changes. MRI may be used to assess cartilage and soft tissues.
- Laboratory Tests: Blood tests and joint fluid analysis can help rule out other conditions like rheumatoid arthritis.
Treatment:
1.Conservative Management:
Weight Management: Reducing weight can decrease joint stress.
Exercise: Strengthening the muscles around the knee, improving flexibility and range of motion.
Physical Therapy: Tailored exercises and modalities to reduce pain and improve function.
Medications: NSAIDs, acetaminophen, and topical analgesics.
Injections: Corticosteroids or hyaluronic acid injections can provide temporary relief.
2.Surgical Options:
Arthroscopy: Minimally invasive surgery to clean out the joint.
Osteotomy: Realignment of bones to offload the affected part of the knee.
Partial or Total Knee Replacement: Replacing damaged parts of the knee with artificial components.


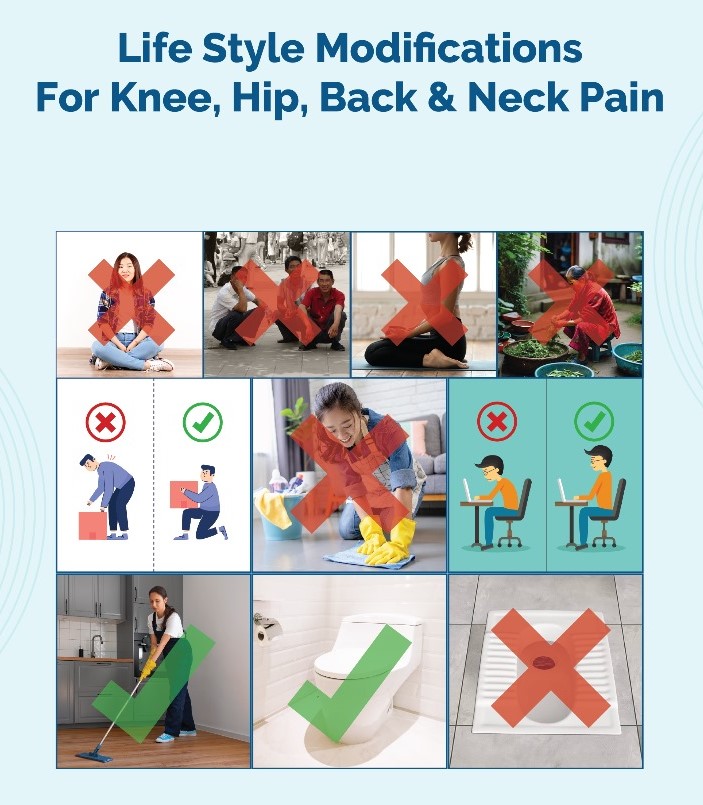
Lifestyle Modifications:
- Activity Modification: Avoiding activities that exacerbate symptoms.
- Supportive Devices: Braces, orthotics, or canes can help reduce stress on the knee.
- Diet: A balanced diet rich in anti-inflammatory foods may help manage symptoms.
Prognosis:
Knee osteoarthritis is a chronic condition, but with appropriate management, many patients can maintain good function and quality of life. Early intervention and a comprehensive treatment plan can help slow disease progression and alleviate symptoms.
When to see a doctor
You should see a doctor for knee osteoarthritis if you experience any of the following:
- Persistent Pain: If you have ongoing knee pain that doesn’t improve with over-the-counter pain medications, rest, or self-care measures.
- Swelling: Noticeable swelling in the knee that doesn’t subside or frequently recurs.
- Stiffness: severe stiffness, especially in the morning or after periods of inactivity, that limits your range of motion.
- Decreased Function: Difficulty performing daily activities, such as walking, climbing stairs, or getting up from a chair.
- Instability: Sensation of the knee giving way or feeling unstable.
- Visible Deformity: Any noticeable changes in the shape or alignment of your knee.
- No Improvement with Self-Care: If lifestyle modifications, such as weight loss, exercise, and home remedies, do not relieve symptoms.
- Interference with Sleep: Pain or discomfort that affects your ability to sleep.
- Other Symptoms: Signs of infection (e.g., redness, warmth, and fever) or other unusual symptoms.
